
No two people have the same skin. That’s why at Total Skin & Beauty Dermatology Center, you’ll always receive a personalized skin damage evaluation. Depending on the condition of your skin, you can choose from a variety of medically approved products, state-of-the-art lasers or minimally invasive surgical procedures. We strive to provide the right procedure for the right individual to ensure that you’ll have healthy, vibrant skin for life.
Common skin conditions
Make your acne problem a thing of the past. If you or your children suffer from acne, you know the physical and emotional problems it can cause. Total Skin & Beauty Dermatology Center offers a comprehensive approach to adult or teen acne. You’ll benefit from a wide variety of treatment methods, including topical prescription medication, antibiotics, acne surgery and new acne laser technologies to treat acne and acne scarring. These therapies are both safe and effective and can make a huge difference in your self-image.



Causes
Acne is a problem caused by inflammation of the pilosebaceous unit of the skin. Just before puberty many hormones develop, some of which stimulate the sebaceous gland to produce more sebum. Sebum can block the opening of the ducts which open to the skin, causing a closed comedone (whitehead). As the gland expands, the duct opens and can become clogged with a dark material causing an open comedone (blackhead). When bacteria fill the ducts of the sebaceous glands, there can be inflammation that causes pustules and nodules. As the inflammation increases, there can be larger nodules and cysts which can lead to scarring.
To some extent acne can be caused by heredity but can also develop in adolescents who have no family history of significant acne. Stress can make acne worse. Many studies have now shown that certain foods once thought to cause acne (chocolate, sodas, caffeine, oily foods) DO NOT cause acne in the vast majority of cases. Acne is NOT caused by poor hygiene.
Treatment
The type of treatment for acne depends on the severity of the acne. Mild comedonal acne (mostly blackheads and whiteheads) is treated with exfoliating cleansers (salicylic acid, glycolic acid) and topical retinoids (adapalene, tretinoin, tazarotene). As more inflammation develops with pustules, papules (red bumps) and nodules, more anti-inflammatory medications are typically added to the regimen. These medications include benzoyl peroxide cleansers and gels, topical antibiotics, and oral antibiotics. Many of our patients will stay on oral antibiotics while they continue to have inflammatory lesions.
When acne is caused by hormonal factors, treatment is often geared toward controlling hormone production. In these circumstances, treatment often includes birth control medication for females or anti-testosterone medication for females (spironolactone).
Isotretinoin is an oral medication used for persistent or resistant acne that doesn’t respond well to more conventional oral and topical therapy. In some cases, acne is so severe with nodules and multiple cysts that Isotretinoin is a first line therapy for adolescent acne.
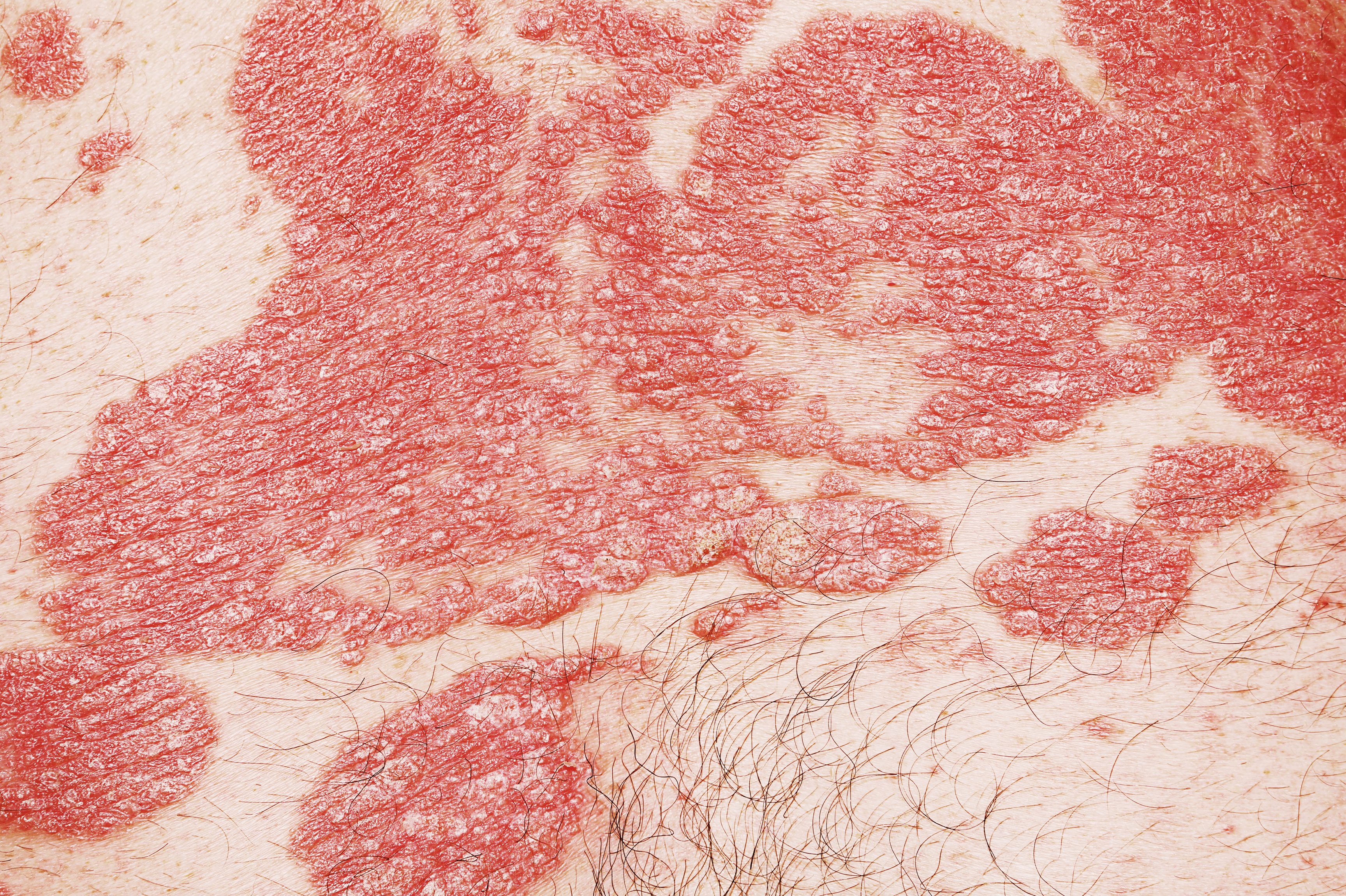
Psoriasis is a common, chronic, non-contagious recurring skin condition consisting of red, scaly, well-defined, thickened areas of varying sizes. Any part of your skin on the body and on your nails can be affected. The scalp, elbows, knees and lower back are commonly affected, but the face is usually not. Arthritis may be associated with your psoriasis.


Causes
The exact cause of psoriasis is unknown, but it is known that psoriasis is an autoimmune condition involving the T-lymphocyte, a type of white blood cell. In psoriasis patients, some parts of the immune system are “turned on” which causes inflammation in the skin and sometimes arthritis. This inflammation causes skin cells to be manufactured and shed much faster than in normal skin. The current theory on treating psoriasis is to reduce the immune reaction that causes psoriasis. In one type of psoriasis (guttate psoriasis) patients will develop their first episode of psoriasis after a bad strep infection.
Arthritis is found in up to 30% of psoriasis patients but in most patients, psoriasis occurs about 10 years prior to the development of psoriatic arthritis. This type of arthritis commonly presents as stiffness in the morning or after long periods in one position (i.e., sitting in a car for long periods). It can also affect the small joints in the fingers, wrists, ankles, or back. In many situations, our psoriasis patients are managed in conjunction with a rheumatologist.
There is new information that suggests psoriasis may be associated with other medical problems including heart disease, obesity, diabetes, and lymphoma. For this reason, we suggest all psoriasis patients keep close follow up with their primary care physicians and live a healthy life style.
Treatment
Systemic and Topical Therapy
We use all systemic and topical therapy for psoriasis including the following internal therapies: Biologic Therapy, Otezla, Methotrexate, Cyclosporine, and Acetretin. We take special care to monitor all appropriate blood work in any patient on these medications. Topical medications we use include topical steroids, topical Vitamin D preparations (sometimes in combination with topical steroids), topical immune modulators (Elidel, Protopic), over the counter tar preparations, and other compounded and non-compounded therapies.
Biologic Therapy
This is the newest systemic therapy for psoriasis. We have been using biologic medications since they were first approved by the FDA for psoriasis in 2003 and have done some of the key pivotal clinical trials for new biologic medications. Our practice has the largest group of patients in Alabama on biologic medications including:
- anti TNF medications (Enbrel, Humira, Remicade, and Cimzia)
- anti-IL 12/23 medications (Stelara)
- anti-IL 17 medications (Cosentyx, Taltz, and Siliq)
- anti-IL 23 medications (Tremfya, Ilumya)
Phototherapy
Phototherapy has been used for psoriasis for more almost 100 years and is extremely safe. We have a large up-to-date phototherapy center with two total body phototherapy units equipped with Narrow Band UVB and UVA lights. We also have a hand/foot unit equipped with narrow Band UVB that is used for patients with difficult hand/foot psoriasis and eczema. We have a full time nurse dedicated to phototherapy and other special psoriasis needs.
Laser Therapy
The Excimer Laser is different from cosmetic lasers that are usually associated with pain during treatment and post-treatment downtime for the patient. Instead, the PHAROS delivers a highly energetic but painless beam of UVB light directly to the psoriasis, vitiligo, and atopic dermatitis patches through a handpiece that rests directly on the patient’s skin. It features the most advanced optical technology on the market, including an adjustable spot size and guiding aiming beam, to target precisely only the affected skin and spare the surrounding healthy tissue from exposure. There is no downtime for the patients.
Patients come in twice each week for an average of 6 weeks, and each quick treatment session that usually takes only 5-10 minutes. Patients usually enjoy several months of treatment-free remission.
Equally exciting for psoriasis patients, the targeted high-dose laser therapy can effectively treat stubborn plaques including knees, elbows, palms, soles, and scalp, even those that have not responded to other treatments.
There are many treatment options for psoriasis that are all available at Total Skin & Beauty Dermatology Center. Patients with localized disease are treated with topical steroid preparations (creams, ointments, foams, solutions, gels), tar preparations, Vitamin D creams or ointments, or with PHAROS laser therapy. More extensive psoriasis is treated with ultraviolet light therapy in our state of the art phototherapy center. Many psoriasis patients are treated with systemic therapy such as Methotrexate, Soriatane, or Cylosporine.
The newest drugs for psoriasis are called biologic medications. These drugs work by suppressing a particular part of the immune system that is most critical for the development of psoriasis. They are all given by injection, either in the office or at home. The current approved biologic medications for psoriasis include Amevive, Enbrel, Humira, Remicade, Stelara, Cosentyx, Taltz, and Siliq. We will work with you to find the most appropriate and safest medication to treat your psoriasis. Total Skin & Beauty Dermatology Center is a regional referral center for psoriasis patients in Alabama and in surrounding states. We encourage our psoriasis patients to join the National Psoriasis Foundation to read more about psoriasis. Also watch an interactive educational video from the National Psoriasis Foundation on causes, types, and treatments of Psoriasis.
Psoriasis Clinical Research Trials
We are frequently involved in clinical research trials for new psoriasis medications. We typically have Phase II, Phase III and Phase IV psoriasis research trials underway. Our psoriasis clinical research unit has been active in trials with Amevive, Enbrel, Humira and other investigational drugs. Call our psoriasis clinical research coordinator to see if any trials might be appropriate for you.
Rosacea is an acne-like condition that occurs on the face, especially the nose, cheeks, chin, and central forehead. It often starts with redness and flushing. Sometimes, these are the only signs a patient may exhibit. However, red bumps (papules), whitish bumps (pustules), and dilated blood vessels (telangiectasias) often also develop. Eyelids will frequently be involved with redness, scaling, and crusting. More rarely, deep bumps can develop in the same areas.
Rosacea is more common in women than men. It occurs commonly in patients in their 20’s and 30’s and peaks during ages 40-60. It rarely occurs in dark-skinned individuals.


Causes
The exact cause of rosacea is unknown. Many theories have been hypothesized including stress, heredity, and gastrointestinal disease, but none of these have been proven. Stress does exacerbate rosacea but is probably not a primary cause. Sunlight, hot (temperature) foods and drinks, alcoholic beverages, and spicy foods are known as tripwires because they may aggravate redness and flushing.
Treatment
Topicals
Topical antibiotics are often prescribed. Erythromycin, clindamycin, and metronidazoles are the ones typically used to treat rosacea. Topical Azelaic acid cream is a new fungal medication used to clear up redness and bumps. Topical antifungal creams will sometimes work in stubborn cases. Occasionally, topical steroid creams can help to cut down the redness and inflammation. Sunscreens are a must because of the role sun often plays in exacerbating rosacea.
Systemic
Oral antibiotics usually work great in rosacea. Tetracyclines (tetracycline, doxycycline, minocycline) typically work best and are usually the first choice. Sometimes, other antibiotics are prescribed. Severe cases may require a more powerful medication called isotretinoin.
Telangiectasias
Dilated blood vessels and diffuse redness can be treated nicely with electrocautery, Diode laser, IPL light treatment or V-beam laser therapy. Usually insurance companies do not cover this treatment.
Eczema is a rash that can be dry or weepy in nature and is typically very itchy. There are many special types of eczema, and they include atopic dermatitis, contact dermatitis, hand eczema, and asteatotic eczema.



Types of Eczema
Atopic Dermatitis
Atopic dermatitis is the name given to a stubborn, itchy rash that occurs in certain persons with sensitive skin. It tends to occur in “atopic” families or those that have members who have asthma, allergies, hay fever, sinus problems, and/or eczema. It usually begins within the first five years of life and may or may not be “outgrown” at adolescence. Certain measures may minimize the risk for breaking out. These include bathing with mild, unscented cleansers and using non-fragranced moisturizers after baths and showers. Any or all of the following may be used in the treatment of atopic dermatitis: topical steroids, systemic steroids, topical or oral immune modulators, oral antihistamines, antibiotics, and phototherapy. Your physician will help guide you with the best treatment for you.
Hand Eczema
Hand eczema can be mild to severe in nature and has many causes. Without proper treatment, hand eczema can become long lasting and can even interfere with normal day to day activities. Treatment involves the use of topical steroids, systemic steroids, topical immune modulators, phototherapy, and sometimes systemic retinoid (derivatives of Vitamin A).
To lesson the risk of hand dermatitis, we recommend protecting hands against harsh soaps, cleansers and other chemicals by wearing gloves. Also, moisturize your hands frequently with a good hand cream after washing and throughout the day.
Asteatotic Eczema
This is dry skin that has become inflamed. It almost looks like a dry cracked lake bed. This is easily treated with topical steroids and good moisturizers.
Contact Dermatitis
This is a rash that occurs from being exposed to a substance that a person is allergic to. The classic example is poison ivy or poison oak. This is best treated with topical and sometimes systemic steroids. There is no shot to prevent breakouts. However, if an exposed person washes the area well within 15 minutes, it minimizes the chance of a breakout.
Dyshidrosis or Dyshidrotic Eczema
This is an inherited form of eczema that is characterized by small blisters along fingers, toes, hands, or feet. Treatment includes topical steroids, systemic steroids, topical immune modulators, phototherapy, and antihistamines, or other oral medications.
Warts are growths on the skin caused by infection with human papillomavirus (HPV). Warts can infect the skin or the mucous membranes of the mouth, nose and genitalia. They are contagious and may spread by direct contact with infected skin. Warts on the sole of the feet are commonly referred to as plantar warts. Multiple small warts are known as flat warts. Genital warts are called condyloma and represent the most common sexually transmitted disease in the U.S. More than 65 different subtypes of HPV have been identified and different subtypes of warts tend to cause different types of lesions. Some HPV types that cause genital warts have a role in the development in some types of cancer such as cancer of the cervix and penis. For this reason, it is important for genital warts to be treated and for females with a history of genital warts to have yearly PAP smears.


Treatment
There is no one best treatment for warts. Treatment options include freezing (cryotherapy), electrosurgery, cantharone (beetle juice), topical medication (aldara, salicylic acid, veregen), injections of bleomycin, and immunotherapy (squaric acid) and in some cases, laser.
There are three main types of skin cancers: basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. All three types of cancers, especially BCC and SCC, can be easily treated with good success if they are caught early.
Basal Cell Carcinoma
Basal cell carcinoma is the most common type of skin cancer and is caused from ultraviolet radiation. It typically occurs on sun-exposed areas: head and neck, chest, back and upper extremities. It often begins as a red or pearly bump; tiny blood vessels are often seen on top of the lesion. Basal cell carcinomas often bleed and look like sores that will not heal.


Treatment
Most BCC’s are treated with surgical excision or Mohs surgery in our office but occasionally superficial BCCs can be treated with topical chemotherapy or superficial radiation therapy.
Squamous Cell Carcinoma
Squamous cell carcinoma is the second most common form of skin cancer. It usually occurs on the head and neck but is also often seen on the back of the hands, forearms, and on the lower legs (especially in older women). SCC is also caused by the sun but is the most common skin cancer seen in patients who a lowered immunity (most commonly from immunosuppressive medications). It presents as a red bump that usually is crusted and looks like it has a scab that won’t heal. Sometimes it has a hard horny cap and can look like a wart.

Treatment
Most SCC’s are treated with surgical excision or Mohs surgery in our office but occasionally superficial BCCs can be treated with topical chemotherapy or superficial radiation therapy.
Melanoma
Melanoma is the most serious form of skin cancer but can be totally cured if discovered at an early stage. The earliest stage of melanoma is called melanoma in-situ. If melanoma is caught in this early stage, it is 100% curable with surgical excision. Deeper, later stage melanomas may be life threatening. It can occur on ANY part of the body (even on the bottom of the feet!) but most melanomas are found on the head and neck, chest, back, and upper extremities. Melanoma is usually pigmented (brown or black) but in rare cases is not pigmented (amelanotic melanoma). Be suspicious of any pigment lesion that grows quickly or develops new dark pigment within a previously existing mole.


Treatment
Most melanomas are treated with surgical excision or Mohs surgery in our office. Please visit our section on Mohs Surgery to learn more.
Actinic keratosis is a common skin disorder that is a consequence of repeated and prolonged exposure to sunlight. It is a thickening of the outer, protective layer of skin, usually forming flat, rough, scaly lesions that may be brownish or somewhat pink in color. The lesions feel rough and may develop a thick, horny surface. Actinic keratoses (plural) usually appear on sun-exposed areas such as the face, ears, neck, chest, backs of hands, and forearms. People who are light haired and fair skinned, who do not tan but burn when exposed to the sun, and spend their lives working outdoors are most likely to develop actinic keratoses.


Treatment
It is important for you to be under the care of a physician, as the lesions of actinic keratosis are premalignant and may develop into skin cancer. Treatment usually involves application of liquid nitrogen, which freezes the lesions causing it to separate from the normal skin underneath. Other treatment options include application of topical anti-cancer drugs, photodynamic therapy, and chemical peels.

